The nurse begins her shift in the intensive care unit. A patient presents with symptoms she hasn't encountered since training three years ago. Protocol has changed since then. The updated guidelines exist somewhere in the hospital's systems, but finding them quickly means navigating multiple databases, checking email attachments, and possibly calling the department head at home. By the time she locates the current protocol, precious minutes have passed.
This knowledge gap repeats thousands of times daily across healthcare organisations. Research from Menlo Ventures demonstrates that healthcare leads all industries in AI in healthcare adoption, with 22% of healthcare organisations implementing domain-specific AI tools in 2025, a sevenfold increase over 2024. More significantly, 70% of healthcare payers and providers are actively pursuing generative AI implementation, recognising both opportunities and challenges ahead.
The urgency driving this transformation proves undeniable. In 2025, 54% of physicians report experiencing burnout, whilst 57% report low well-being. Administrative overhead continues eroding margins, and hospital digital transformation faces mounting pressure as healthcare data volumes exceed 10 trillion gigabytes. AI knowledge platforms address these challenges by transforming how healthcare teams access and act on critical information.

Healthcare organisations face distinct knowledge management challenges that differ substantially from other industries. Understanding these structural issues clarifies why AI for clinicians and administrative staff proves particularly valuable.
Medical knowledge evolves at unprecedented pace. Treatment guidelines update continuously. New research emerges weekly. Regulatory requirements shift quarterly. Medications receive updated warnings. Procedures gain refined protocols. Individual clinicians cannot possibly maintain current knowledge across all domains through memory alone, yet patient safety depends on applying the most recent, validated information.
Staff turnover compounds knowledge retention challenges. Healthcare experiences chronic workforce shortages. When experienced nurses and clinicians leave, institutional knowledge disappears with them. New staff require months to achieve full competency, during which knowledge gaps create risk. Traditional onboarding processes cannot keep pace with turnover rates whilst maintaining rigorous safety standards.
Fragmented information systems create operational friction. Clinical guidelines reside in one system. Medication protocols live in another. Administrative procedures occupy separate databases. Patient records require different access. Policy updates arrive via email. Critical information becomes trapped in silos, forcing healthcare professionals to hunt across multiple systems whilst patients wait.
High patient loads eliminate time for knowledge seeking. Emergency departments operate at capacity. ICU nurses manage multiple critical patients simultaneously. Primary care physicians see patients in rapid succession. The time available to search through documentation, verify protocols, or consult reference materials simply doesn't exist during active patient care. Healthcare professionals need answers immediately or make decisions with incomplete information.
Fast-changing guidelines create compliance challenges. Regulatory requirements from bodies like the CQC evolve regularly. Clinical knowledge platforms must reflect current standards to maintain accreditation. Outdated protocols create liability exposure. However, ensuring all staff remain current on every guideline proves extraordinarily difficult with traditional training approaches.
Research from the National Library of Medicine emphasises that healthcare providers spend significant time managing health records and documentation. Because much of this data remains unstructured, excessive time gets consumed by note-taking and information retrieval rather than direct patient care. This administrative burden directly contributes to clinician burnout and reduces time available for patient interaction.
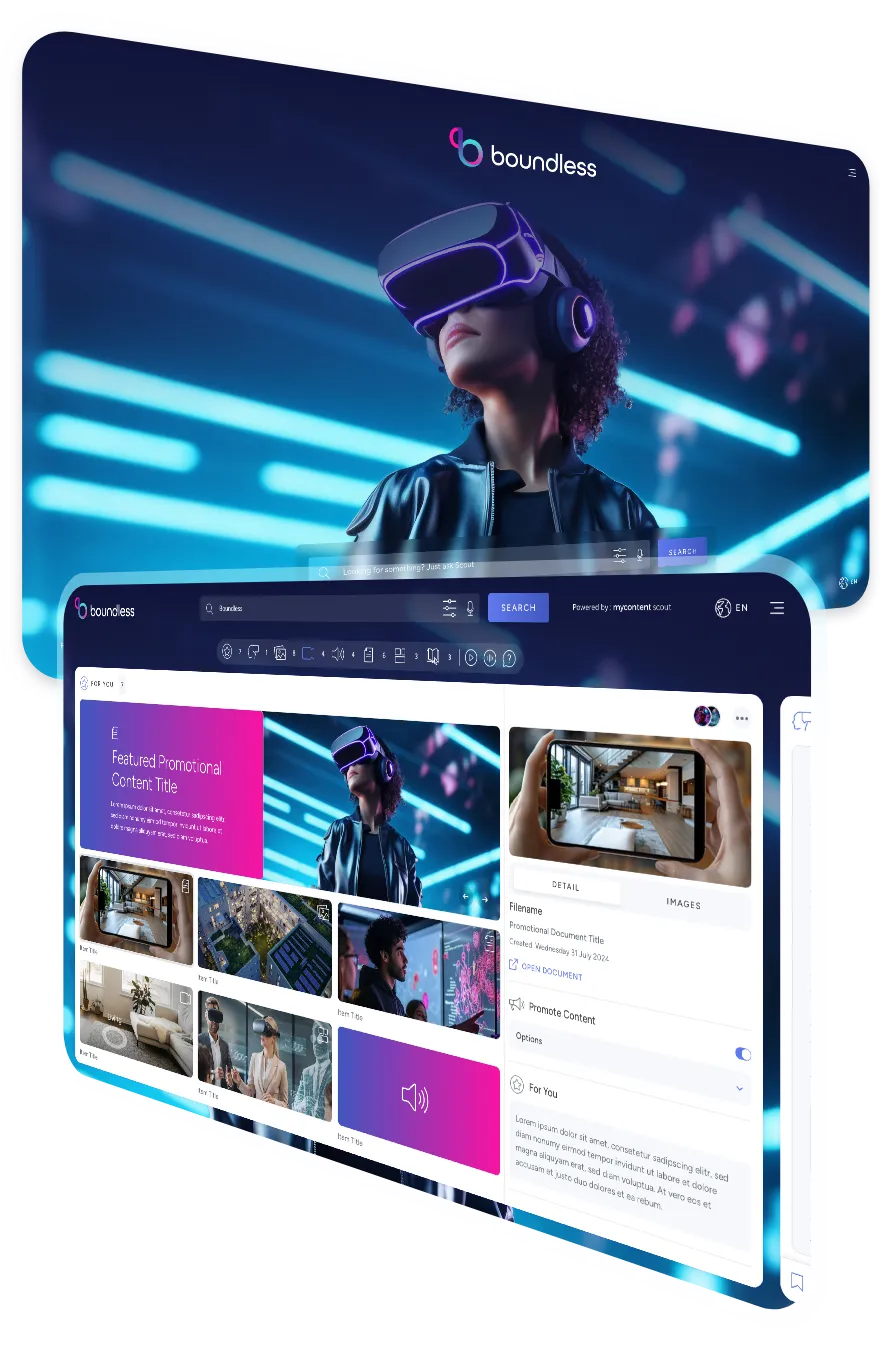
AI-powered platforms like MyContentScout transform knowledge access across healthcare organisations by providing role-specific support tailored to how different professionals actually work.
For clinicians, the platform delivers instant access to medical knowledge exactly when needed. A physician treating a patient with unusual symptoms can query the system in natural language: "What's the current protocol for managing acute kidney injury in patients with diabetes?" The AI immediately surfaces the latest clinical guidelines, relevant research, and internal hospital protocols specific to that condition. Rather than interrupting patient care to search through documentation, clinicians receive validated information within seconds.
The platform goes beyond simple retrieval. It understands clinical context, recognises relationships between conditions, and surfaces information about drug interactions, contraindications, and alternative treatments. When guidelines change, the system ensures clinicians access current protocols rather than outdated information that might compromise patient safety.
For nurses, quick reference capabilities prove transformative. Nurse onboarding AI accelerates the journey from newly hired to fully competent. New nurses can instantly access step-by-step procedures for tasks they haven't yet mastered: administering specific medications, operating equipment, following infection control protocols, or managing emergency situations. Rather than repeatedly asking senior staff or hunting through procedure manuals, they get immediate, accurate guidance.
Experienced nurses benefit equally. When patient situations require procedures outside their typical practice, the system provides instant protocol access. Managing a patient with a PICC line whilst your usual assignment involves post-surgical care? The platform delivers current evidence-based guidelines immediately. This capability proves particularly valuable in smaller facilities where specialised expertise isn't always available on every shift.

For HR and administrative teams, the platform streamlines onboarding, compliance training, and operational guidance. New employee onboarding traditionally consumed weeks of HR time: scheduling training sessions, tracking completion, ensuring regulatory compliance, and maintaining documentation. AI platforms automate substantial portions of this process whilst improving consistency and thoroughness.
New staff members access role-specific onboarding materials at their own pace. The system tracks completion, tests comprehension, and ensures all mandatory training gets completed before independent practice begins. Compliance requirements for topics like infection control, HIPAA, safeguarding, and emergency procedures get standardised across all staff, reducing variability that creates risk.
Administrative guidance becomes equally accessible. Questions about payroll procedures, scheduling policies, benefits enrolment, or facility protocols receive immediate, consistent answers. Rather than waiting for HR availability or searching through policy documents, staff get accurate information instantly. This reduces administrative bottlenecks whilst improving employee satisfaction.
The platform integrates across existing systems rather than replacing them. It connects to electronic health records, policy databases, training systems, and clinical guidelines, creating a unified interface for knowledge access without requiring organisations to abandon established infrastructure. This integration approach accelerates adoption whilst reducing implementation complexity.
Consider a district hospital that implemented MyContentScout to address persistent challenges with nurse onboarding and patient safety AI tools. Previously, their onboarding process required six weeks before new nurses worked independently, during which time they required constant supervision that stretched experienced staff thin.
The hospital faced several interrelated problems. High turnover created constant pressure to hire and train new nurses. Knowledge gaps during the learning period occasionally resulted in errors that triggered incident reviews. Experienced nurses spent excessive time answering repetitive questions from trainees rather than focusing on patient care. The onboarding burden made shifts stressful for everyone whilst patient care quality occasionally suffered.
After implementing the AI knowledge platform, the hospital redesigned its onboarding approach. New nurses received structured digital learning paired with practical experience. The platform provided instant access to protocols, procedures, and clinical guidelines throughout their shifts. When encountering unfamiliar situations, they could query the system immediately rather than searching for a supervisor.
For example, a newly hired ICU nurse encountered a patient requiring specific wound care she hadn't performed since training. Rather than locating a senior nurse who might be managing a critical situation with another patient, she queried MyContentScout: "What's the current protocol for negative pressure wound therapy?" The system immediately provided step-by-step instructions, equipment requirements, contraindications to watch for, and documentation requirements. She completed the procedure correctly and confidently without interrupting colleagues.
The impact proved substantial across multiple dimensions. Onboarding time reduced by 40%, with new nurses achieving independent practice competency in 3.5 weeks rather than 6 weeks. This acceleration didn't compromise safety; in fact, incident reports related to knowledge gaps decreased by 60% during the first year after implementation. The reduction stemmed from new nurses having immediate access to correct protocols rather than relying on memory or interrupting busy colleagues.
Patient safety metrics improved measurably. Medication administration errors declined by 35%. Protocol compliance increased significantly, particularly for time-sensitive interventions like sepsis management where minutes matter. Patient satisfaction scores rose as nurses spent more time on direct care rather than searching for information or tracking down senior staff for guidance.
Staff satisfaction improved equally. New nurses reported feeling more confident and supported during their learning period. Rather than feeling foolish for not knowing something, they could quietly check the platform and proceed confidently. Experienced nurses appreciated reduced interruptions, allowing them to maintain focus on their patients. The overall ward atmosphere became less stressed as knowledge barriers decreased.
Financial implications proved compelling. Faster onboarding meant new nurses contributed productively sooner, reducing the effective cost per hire. Lower error rates meant fewer incident investigations and reduced liability exposure. Higher staff satisfaction translated to improved retention, with turnover decreasing by 22% in the year following implementation. These combined benefits delivered return on investment within 14 months.

Healthcare AI implementations demand rigorous attention to healthcare data security and compliance. The sensitivity of medical information and strict regulatory requirements make security foundational rather than supplementary.
HIPAA compliance represents the baseline requirement for any healthcare AI system operating in the United States. The Health Insurance Portability and Accountability Act establishes comprehensive standards for protecting patient health information. AI systems that process protected health information (PHI) must comply with both the Privacy Rule governing how PHI can be used and disclosed, and the Security Rule requiring administrative, physical, and technical safeguards.
HIPAA compliance for AI introduces specific challenges. The Privacy Rule's minimum necessary standard requires AI tools to access only PHI strictly required for their purpose, even though AI models typically seek comprehensive datasets for optimal performance. De-identification becomes critical when training models, but organisations must ensure de-identification meets Safe Harbor or Expert Determination standards whilst guarding against re-identification risks.
Business Associate Agreements (BAAs) with AI vendors prove essential. Any AI vendor processing PHI must operate under robust BAAs outlining permissible data use and required safeguards. According to HIPAA Journal guidance, generic AI tools like standard ChatGPT cannot be used with PHI because providers don't sign BAAs. Healthcare organisations must specifically select HIPAA-compliant AI platforms designed for healthcare use.
Role-based access controls ensure that AI systems surface only information users are authorised to access. Not everyone should see all patient data, clinical guidelines, or administrative information. Junior nurses require different access than department heads. Administrative staff shouldn't access clinical records. Financial personnel need budget information but not treatment protocols.
MyContentScout implements granular permission systems that respect these boundaries. When a nurse queries about a patient protocol, the system confirms the nurse has appropriate access before providing information. When administrative staff search for policy information, they receive relevant guidance without exposure to clinical data. These controls operate transparently, maintaining security without creating friction for legitimate access.
Audit logs and traceability address both regulatory requirements and operational needs. Healthcare organisations must demonstrate compliance with privacy regulations, requiring comprehensive records of who accessed what information and when. Audit trails also prove essential for incident investigation, quality improvement, and identifying training needs.
The platform automatically logs every query, response, and access event. If questions arise about whether a staff member had access to appropriate information during a patient care situation, complete records exist. If privacy concerns emerge, administrators can trace exactly what information was accessed and by whom. This transparency builds trust whilst satisfying regulatory requirements.
Validated, trustworthy sources prevent AI from providing inaccurate or outdated information that could compromise patient safety. Not all information deserves equal weight. Peer-reviewed clinical research, official treatment guidelines, and hospital-approved protocols represent validated knowledge. Blog posts, social media content, and non-peer-reviewed sources do not.
MyContentScout curates its knowledge base carefully, incorporating only validated clinical information from authoritative sources: NICE guidelines, peer-reviewed medical journals, official hospital protocols, regulatory requirements, and manufacturer specifications for medical devices and medications. The system clearly cites sources for every piece of information provided, enabling users to verify provenance and currency.
When guidelines update, the platform reflects changes immediately rather than continuing to provide outdated information. Version control ensures that audit trails capture which version of protocols was current when specific decisions were made, addressing liability concerns whilst supporting continuous improvement.
Looking ahead, AI workflow automation in hospitals continues evolving in ways that promise even greater impact on patient care and operational efficiency.
Integrated workflows across departments represent the next evolution. Rather than isolated tools for specific functions, AI platforms will coordinate information flow across the entire patient journey. When a patient arrives in A&E, the system can immediately surface relevant medical history, current medications, known allergies, and recent test results for the treating physician. When that patient moves to a ward, nursing protocols tailored to their specific conditions become instantly available. When discharge planning begins, the platform provides appropriate patient education materials and follow-up requirements.
This integration extends beyond clinical care to administrative processes. Bed management, staffing allocation, supply chain logistics, and billing processes all benefit from AI coordination. The platform recognises patterns: certain conditions typically require specific resources, enabling proactive allocation before bottlenecks occur. Operating theatre scheduling optimises based on procedure types, surgeon availability, and equipment requirements.
Real-time updates for guidelines and policies ensure organisations remain current without manual intervention. When NICE updates treatment guidelines, when regulatory requirements change, or when hospital policies evolve, the platform updates immediately. All staff access current information automatically without requiring retraining sessions or email announcements that often go unread.
This real-time updating proves particularly valuable during public health emergencies. When COVID-19 protocols changed frequently, organisations struggled to ensure all staff remained current. AI platforms can push critical updates instantly, ensuring consistent application of new protocols across all shifts and departments simultaneously.
AI-powered decision support for complex cases augments clinical judgement in situations involving multiple interacting factors. A patient with diabetes, heart disease, and kidney impairment presents medication management challenges where interactions and contraindications require careful balancing. AI can analyse the complete clinical picture, flagging potential issues and suggesting evidence-based approaches whilst leaving final decisions to clinicians.
This support extends to diagnostic assistance. AI systems analysing symptoms, test results, and medical history can suggest differential diagnoses that clinicians might consider, potentially identifying rare conditions that might otherwise be overlooked. The technology augments rather than replaces clinical judgement, serving as a safety net that catches potential oversights.
Continuous learning systems that adapt improve over time based on usage patterns and outcomes. The platform recognises which queries occur frequently, identifying potential training needs or documentation gaps. When users repeatedly search for the same information, it suggests creating quick-reference materials or improving protocol visibility. When certain procedures consistently trigger questions, it indicates opportunities for enhanced training.
The system also learns from clinical outcomes, though always with appropriate oversight and validation. If particular treatment approaches consistently produce better results, the platform can surface relevant evidence to clinicians. If certain error patterns emerge, it can proactively provide additional guidance to prevent similar issues.

The evidence demonstrates conclusively that AI knowledge platforms deliver measurable improvements in patient care, staff satisfaction, and operational efficiency. Healthcare organisations implementing these capabilities position themselves to address mounting pressures facing the sector whilst improving outcomes for patients and staff alike.
The transformation extends beyond technology implementation. It represents fundamental reimagining of how healthcare organisations manage and disseminate knowledge. Rather than accepting that critical information remains scattered and difficult to access, progressive organisations recognise that instant access to validated knowledge enables better decisions at every level.
Staff benefit through reduced cognitive load and enhanced confidence. Rather than making decisions with incomplete information or interrupting colleagues for guidance, they access comprehensive, current knowledge instantly. This support proves particularly valuable for newer staff still building expertise and for experienced professionals encountering situations outside their typical practice.
Patients benefit through safer, more consistent care delivery. When every clinician can instantly access current protocols, evidence-based guidelines, and relevant patient information, care quality improves. Errors decrease. Treatment follows best practices more consistently. Patient education becomes more comprehensive and accurate.
Organisations benefit through operational efficiency and reduced liability. Onboarding accelerates. Compliance improves. Documentation becomes more thorough and consistent. Error rates decline, reducing both human suffering and financial exposure. Staff retention improves, decreasing recruitment costs and maintaining institutional knowledge.
At The Virtual Forge, we help healthcare organisations implement AI knowledge platforms that transform how teams access and act on critical information. Our approach recognises that healthcare implementation requires understanding both technical capabilities and clinical workflows, ensuring solutions integrate seamlessly into existing practice whilst meeting rigorous security and compliance requirements.
We begin by assessing your organisation's specific knowledge management challenges: where information currently lives, how staff access it, where friction impedes care delivery, and which use cases would deliver the greatest impact. This assessment identifies opportunities to improve patient safety, enhance operational efficiency, and support staff satisfaction through better knowledge access.
Our implementation expertise ensures platforms integrate with existing EHR systems, policy databases, and training platforms without requiring wholesale replacement of established infrastructure. We design solutions that respect clinical workflows rather than disrupting them, ensuring adoption occurs naturally because the platform genuinely makes work easier rather than adding burden.
Security and compliance receive rigorous attention throughout. We ensure HIPAA compliance, implement appropriate access controls, establish comprehensive audit trails, and validate that only trustworthy, current information reaches users. These foundations prove essential for healthcare applications where errors can harm patients and regulatory violations carry serious consequences.
Training and change management support successful adoption. Technology alone delivers minimal value without ensuring staff understand how to leverage it effectively. We develop customised training programmes addressing different roles, facilitate champion networks within departments, and provide ongoing support as the platform evolves.
Whether you're exploring AI knowledge management for the first time, struggling with existing implementations that underdeliver, or scaling successful pilots across your organisation, we're here to help.
Ready to give your healthcare teams instant access to validated knowledge? Contact us to explore AI knowledge platforms tailored for hospitals and clinics. Our team can assess your specific challenges and design solutions that improve patient care whilst supporting your clinical and administrative staff.

Get in touch with our team to arrange a demo of MyContentScout and see how it could transform your workflow with AI search, content analysis and categorisation, saving you time and providing smart insights from various sources.